PCOS Signs And Symptoms
PCOS Ovaries
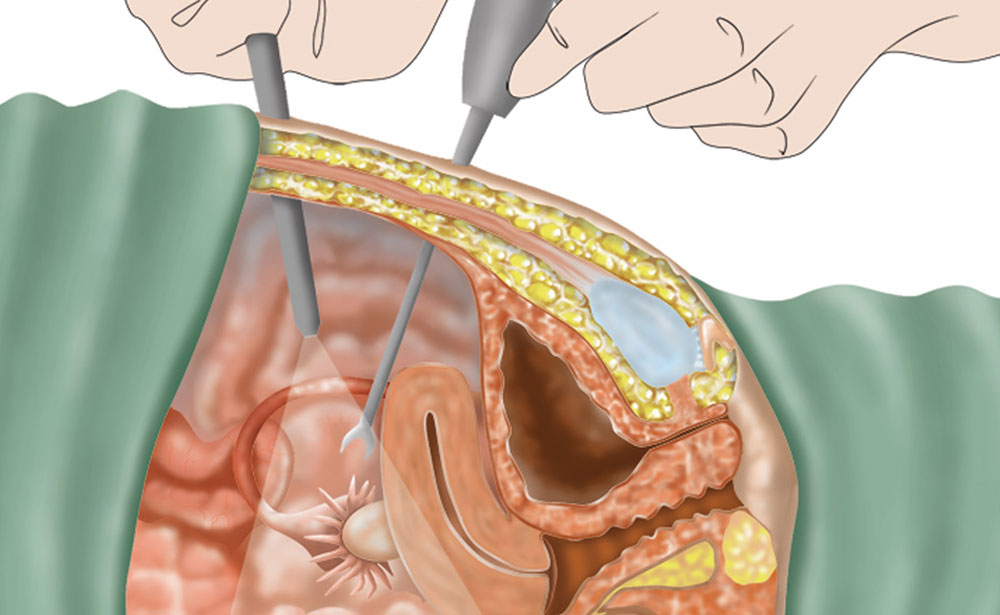
Polycystic ovaries are defined as enlarged ovaries with multiple small follicles. If there are 12 or more follicles in each ovary, this is classified as PCOS. Women with PCOS usually present with enlarged ovaries with numerous enlarged peripheral cystic follicles and increased central stroma (the middle section of the ovary which produces androgens). Many studies suggest that the polycystic appearance is due to increased production of androgens, which leads to lack of ovulation resulting in the follicle atresia (arrest of development).
Many of the cysts that occur in a polycystic ovary are follicles that will eventually mature to produce an egg, but due to abnormal hormone levels, have never ovulated. The term polycystic ovaries does not imply that the ovaries contain many cysts, it only refers to the ultrasound finding of ovaries with many small follicles (usually 12 or more) in each ovary.

Amenorrhea( Irregular Menstrual)
Polycystic ovaries are defined as enlarged ovaries with multiple small follicles. If there are 12 or more follicles in each ovary, this is classified as PCOS. Women with PCOS usually present with enlarged ovaries with numerous enlarged peripheral cystic follicles and increased central stroma (the middle section of the ovary which produces androgens). Many studies suggest that the polycystic appearance is due to increased production of androgens, which leads to lack of ovulation resulting in the follicle atresia (arrest of development).
Many of the cysts that occur in a polycystic ovary are follicles that will eventually mature to produce an egg, but due to abnormal hormone levels, have never ovulated. The term polycystic ovaries does not imply that the ovaries contain many cysts, it only refers to the ultrasound finding of ovaries with many small follicles (usually 12 or more) in each ovary.

Acne / Thinning Hair / Hirsutism
Acne can occur at any age and it is often due to excess androgens. Oral contraceptives in combination with antibiotics can be effective. Accutane has been used with varying degrees of success.

Thinning hair
Hair loss around the scalp is called androgenic alopecia and is due to an increase in androgens causing hair thinning. Several combination treatments must be utilized to minimize hair thinning, including combination of oral contraceptives and spironolactone. Minoxidil or Rogaine have been moderately effective in growing hair and must be used continuously. Retin-A may also be effective alone or in combination with Rogaine.

Excess Body Hair (Hirsutism)
Hirsutism is present in approximately 25% of women and in about 70-80 % in women with the diagnosis of Polycystic Ovarian Syndrome. Hirsutism may signal underlying endocrine or metabolic abnormalities, such as androgen excess and PCOS. Other signs of elevated androgens include hair loss, irregular menses, acne, acanthosis nigricans (skin condition), and others. Approximately 5-15 % of women with hirsutism have no identifiable underlying cause.
Hirsutism is often due to elevated ovarian testosterone, which leads to thinning of the scalp hair while increasing facial and abdominal hair in women. High levels of testosterone can result in lowering of the voice, classic “pear shaped” body appearance, irregular (or no) ovulation, and other symptoms.
Normalization of testosterone levels can often be achieved by using a combination of oral contraceptives and Aldactone (spironolactone), a diuretic that also decreases androgen production.
All patients with hirsutism should undergo a physical and laboratory examination, which includes menstrual history, evaluation of progression of hair growth, and review of current medications.
The laboratory evaluation should include thyroid hormones, prolactin levels, fasting insulin, glucose levels, free testosterone, DHEAS, 17-hydroxprogesterone and sex hormone binding globulin. These laboratory fertility tests are typically performed in the morning before day 8 of the menstrual cycle.
> Oral contraceptives alone or in combination with Aldactone (spironolactone) work well to decrease the growth of new hair.
> Vaniqa-A cream applied twice daily may decrease hair growth after only 8 weeks of therapy.

> Electrolysis is effective for permanent hair removal; involves insertion of sterile probes into the hair shaft followed by heat and/or chemical treatment. This necessitates frequent sessions and multiple treatments per follicle. Scarring, hypopigmentation, and skin puckering can result if not performed correctly.
> Laser hair removal uses treatment principals similar to electrolysis but with quicker and more effective long-term results. The laser utilizes light to heat melanin (the pigment in the hair) so the hair and the surrounding follicle structures are damaged and destroyed, sparing the skin.
> Shaving or clipping with scissors is the fastest temporary hair removal method and will not promote hair growth.
PCOS Weight Loss & Nutrition
Many women with polycystic ovarian syndrome (PCOS) struggle with their weight. Women with PCOS often find it difficult to lose weight even with dramatic decreases in their food intake. They are at high risk for impaired insulin metabolism and diabetes. Studies have shown that lower carbohydrate (41% vs 55%) diet resulted in lower fasting glucose, lower fasting insulin, and lower testosterone. Tweezing and waxing are the worst techniques producing thicker, darker, and denser follicles. Also the skin may develop acne, ingrown hairs, folliculitis, and scarring.
What is Body mass index (BMI)?
> BMI is a measure of body fat based on height and weight.
> BMI is a better predictor of disease risk than body weight alone. However, there are certain people who should not use BMI as the basis for estimating body fat content. Examples include: competitive athletes and body builders, whose BMI is high due to a relatively larger amount of muscle, and women who are pregnant or lactating. BMI is also not intended for use in growing children or in frail and sedentary elderly individuals.
If your BMI is high, you may have an increased risk of developing certain diseases, including:
> Hypertension(high blood pressure): women with PCOS often suffer from high blood pressure
> Cardiovascular disease: there is substantial evidence that the increased lipids, insulin resistance, and hypertension can result in an increase in cardiovascular disease. The following factors are found in patients with PCOS:
Increased CRP (C-reactive protein is a marker of inflammation and correlates with the risk of cardiovascular disease)
Increased coronary artery (vessels feeding the heart) calcium, which can increase the risk of heart disease
Increased carotid intima-media thickness (vessels which supply the brain), which can increase the risk of stroke
> Dyslipidemia includes elevation of cholesterol/triglycerides is seen in 70% of women

> Adult-onset diabetes (Type II)
> Sleep apnea: may be caused by insulin resistance in the system or an increased body mass index. Fatigue is just as common and may be related to insulin resistance or low thyroid function (hypothyroidism), either of which can cause reduced energy levels. (Link to remedies) Salivary testing- Sleep 360, or visit Lisanne wellness center
> Osteoarthritis
> Female infertility seen in 55-75%
Prevention of further weight gain is important and weight reduction is desirable.
At Lisanne wellness center as part of PCOS management they will test your BMI to get an accurate assessment.
· Insulin resistance is estimated to be present in 80% of patients and obesity increases the incidence of insulin resistance.
PCOS Weight Loss & Nutrition
Insulin resistance is diagnosed in cases then the glucose to insulin ratio is greater than 4.5, the 2-hour glucose levels are greater than 140 mg/dL, or if fasting insulin is greater than 10 µIU/mL.
Progressive insulin resistance will eventually lead to exhaustion of the cells of the pancreas and the development of diabetes mellitus ensues.
Insulin resistance and the risk of diabetes can be resolved through careful lifestyle modification with an appropriate diet and an exercise program.
Acanthosis
Nigrican
Depression, Anxiety and
Mood Swings
It is not clear whether depression and/or anxiety are due to the hormonal imbalances seen in PCOS or to the impact of the symptoms (weight gain, excessive hair growth, acne, and infertility) in self-esteem and quality of life. Nonetheless, many women with PCOS experience one or both problems.
Some women experience improvements in depression and anxiety when insulin/glucose metabolism problems are address with diet, exercise, and sensitizing medications. Other women require the use of antidepressants along with diet and exercise to improve symptoms.
Thyroid
Disorders
Studies show a link between PCOS and an under-active thyroid, a condition known as hypothyroidism, Hashimoto’s Disease, or chronic lymphocytic thyroiditis. For this reason, women who have been diagnosed with PCOS should undergo routine thyroid function testing.
· Metabolic Syndrome: a combination of various metabolic conditions. The syndrome is diagnosed when a patient meets three or more of the following criteria:
· Blood pressure: 130/85 mm Hg or higher
· Triglyceride levels: 150 mg/dL or higher
· HDL-cholesterol levels: less than 50 mg/dL
· Abdominal obesity: waist circumference greater than 35 inches
· Fasting glucose: 110 mg/dL or higher